Three Futures for Medicine
The Cure in the Code by Peter Huber
The Creative Destruction of Medicine by Eric Topol
- ... and mine
Two books about the future of medicine. I am ideologically libertarian; to me that means freedom for as many people as possible, including those who own corporations (everyone with a pension fund), work for them, and buy from them. Huber's book seems focused on pharmaceutical corporations, accepting unquestioningly that wide sales for their products are in everyone's best interest. Topol's book focuses on digital medicine, where biology plus genome plus information technology is in everyone's best interest. Mostly missing from both books is the idiosyncratic human being we call a "patient", their journey out of acute illness, and the doctors who can guide them. Also mostly missing is clinical discovery; in spite of giant research programs, most new discoveries in medicine is made by individual doctors and researchers following up on unexpected observations.
That said, both books provide useful information; along with Morton Meyers' Happy Accidents and Roger Williams' Biochemical Individuality, they help us understand where "medicine as if people matter" is going, and where it should go (not the same thing).
80% of the damage walking in a clinic's front door is self-inflicted; much of that due to the television lifestyle, much from avoidable accident and ignorance. Sometimes a doctor can guide and accelerate nature's healing process, and sometimes a doctor can help mask the unavoidable symptoms. But the body does the healing, and the body cannot completely heal after most kinds of damage. A doctor's most important task is advising patients to mindfully protect their own health, and in a 30 minute visit once a year, counteract thousands of hours of bad advice from media, friends, and family. Far better to avoid damage in the first place, than try to fix it afterwards.
Both Huber and Topol disparage FDA mass medicine at the dawn of genomics. Roger Williams pointed out in 1956 that people vary widely; a "standard" blood test focuses on those few measurements that are repeatable across many people, not the ones most indicative of individual health. We target mass therapies like statins and weight loss on easy-to-make measurements like LDL cholesterol and body mass index, and their deviation from whole-population averages, rather than the optimum for each person's genome and situation. Thus, my insurance company will penalize my doctor because my LDL cholesterol is high, even though my blood pressure and cardiovascular health is excellent. I refuse to take statins, because they hurt, and because the mevalonate pathway that they interrupt is vital to brain health and the synthesis of dozens of important sterols. But my doctor already struggles financially, even though the important advice and clinical judgement he offers isn't available from algorithms, pill factories, and paraprofessionals.
Craig Venter, whose team accelerated the sequencing of the first human genome, said he couldn't determine his eye color from his genome. The exome is a protein recipe book, the introme is timing, and a body develops from those instructions, the environment, and accident. A genome can tell us whether a pharmaceutical might find a target protein to latch onto, and this is important information for therapy. But this maybe is overshadowed by is, the actual patient response, and that is a complex matter of history, circumstance, attitude, and perception. If the diagnostic equipment says "healthy" and the patient says "sick", they still need healing, and whether that healing comes from drugs, teaching, situation change, or just an attentive ear and ally, there are some complicated and experience-driven judgements to make and actions to take. Holistic medicine is a label misapplied to lots of woo-woo nonsense, but in the end it recognizes that people have brains and "souls" (patterns of mind) as well as bodies. Medicine that ignores this can be expensive torture,
Huber goes on about the importance of "intellectual property". Pharmas spend billions of dollars developing their molecules and proving them to the FDA's satisfaction. They must do so in secret, or they lose competitive advantage. So, apparently, we should spend lots of money on pills, and suppress knockoffs. But what if this development model is criminally insane? Innovation occurs when seemingly unrelated ideas combine in one human brain, and sequestered minds don't encounter enough unrelated ideas. Development involves many minds, but as we say in open source, "the best minds don't work here". In our internet connected age, drug development can occur in many cooperating and competing places, with a picture emerging from all of them; trials can also be public, based on volunteers, and other volunteers can help the general public understand the results. This does not have to cost billions or even millions of dollars from any one organization. The FDA's 21st century role should not be gatekeepers. They should focus on diseminating information that helps individuals and their doctors and advisors make their own decisions, and let us know what the results of those decisions are. Reducing this process to a single "permit or deny" decision produces the least information and the most expensive binary bit imaginable.
A companion organization to the FDA, under the Department of Justice, should seek out and prosecute those who fraudulently provide demonstrably damaging misinformation about drugs and cures. People make mistakes, and some individuals are stubborn about repeating them. These are not crimes, and nature provides ample punishment. We should know about those natural punishments, we do not need a government agency adding to them. However, when someone makes a bad decision because they are lied to, we may need to punish the liars, if that is what it takes to stop them. First, though, we should "out-inform" the crooks with better information.
This is why I like Topol's book better. In Topol's future, patients will use their genomics, and the medical history in their electronic records, and floods of information from body sensors, to make good decisions with the help of professional healers.
This is a time consuming process; while a healer's task can theoretically be accelerated with electronic tools, electronic communication takes time, is fraught with risk, and is poorly compensated. Topol is no longer a primary care physician, he attributes doctor's reluctance to use email to technophobia. In fact, carefully composing an email to a patient that is both accurate and effective is a very difficult task. Far more difficult than sending out an appointment reminder or scheduling a meeting, and the latter can cost a busy executive a large part of an hour. Imagine individual email correspondence with 2000 patients - that could be 10 full time jobs, not a part time activity for one clinic. Kaiser demands that their doctors answer email, and they do so all week, day and night; the old job of diagnosis and cure occurs on weekends. Communication mistakes can kill. I've used email for three decades, and seen much miscommunication and angry escalation between healthy people. I cannot imagine making life-changing announcements and providing careful instructions this way.
All that said - Topol tells us about emerging technologies that intelligent and engaged people will learn how to incorporate in their lives. It was great learning about 23andMe, and the Trait-o-Matic interpretation software that George Church maintains at Harvard. On page 23 of the first paperback edition, Topol shares the excellent phrase "eminence-based medicine", where authoritarian bluster substitutes for a paucity of clear facts.
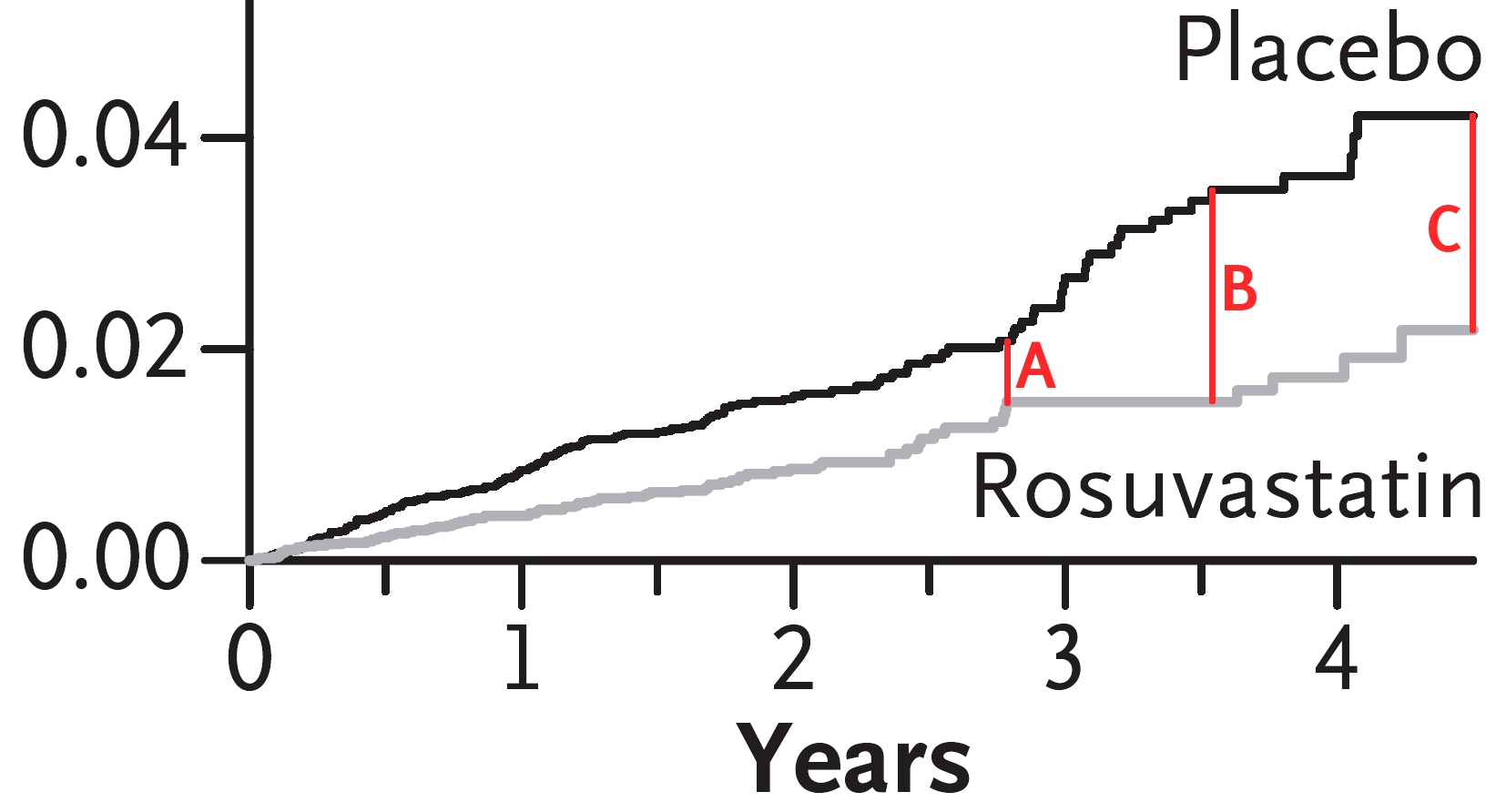
Cardiology-trained Topol does engage in "eminence" himself. On page 22, he shows a graph for rosuvastatin, the outcomes for Crestor versus placebo for patients with high C-reactive protein. The graph does NOT show $6/pill Crestor/rosuvastatin versus off-patent $0.33/pill atorvastatin or $0.51/pill pravastatin, nor does it show patients with low C-reactive protein like myself after diet and exercise improvements. It does not differentiate between death, heart attack, and stroke - all can be due to infarction, but the differences in each separate category may vary. The most interesting thing about the graph is that it is cumulative, rather than per year; at 2.75 years, the lines converge a bit, then spread out at 3.5 years, then seem to track each other after that. That strongly demonstrates the effect of the choice of trial termination time, a source of possible fraud in Astra-Zenica's Jupiter trial.
Death certificates are not scientific documents, they are the opinions of the physician present when a person dies, and most people die for more than one reason, and most doctors are influenced by advertisements. Statins certainly do reduce serum cholesterol, and if a patient's heart stops and their cholesterol is known to be high, it is pronounced as a heart attack, probably without autopsy. If the patient has a stroke and their cholesterol is high, that is pronounced as ischemic stroke, and nobody will bother to spend thousands of dollars on an MRI or autopsy to find out that it is intracerebral hemorrhage instead. Those graphs have a large subjective component, one that statin manufacturers can manipulate.
So - enjoy Topol, but remember that his opinion is colored by his specialization and his love of technology.
|
A strange graph reproduced as figure 2.1 in Topol. At (A), the differences between placebo and rosuvastatin is about 25%. Note the sudden change in both slopes. At (B), the difference has jumped to 100%, entirely because of a big jump in the placebo group, and 9 months of zero deaths in the rosuvastatin group. WTF? Have all the bad outcomes been shifted to the control group??? At (C), the difference is the same as (B); both graphs have followed the same average slope. The Jupiter trial was plagued with methodological and statistical shenanigans that some consider fraud. |